One of the most frequent complaints of children brought to an emergency room or urgent care facility is rashes. While most rashes are benign and need minimal intervention there are some that are very dangerous and need immediate medical care.
The first rule of thumb that I use when a parent calls to say that a child has a rash is that rashes must be seen and not described. It is difficult to diagnose a rash if the parent describes it on the phone. The second rule of thumb is fever. If a child is in any distress s/he must be seen immediately no matter what the rash looks like or whether the child has fever.
The description of rashes is somewhat confusing because most are described with Latin words. An example is a red rash described as erythematous; a raised rash is papular rash, and a macular rash is a spotty rash. None of these terms indicates cause or severity, just a description. The most common presentation is a maculapapular rash, which means a blotchy, red, raised rash.
A frequent complaint is a rash which appears a day or two after being in the outdoors. Parents will frequently call and say they know this rash is poison ivy and could we prescribe something over the phone. Poison ivy is actually a contact dermatitis secondary to a reaction to a resin which is present in the plant. “Contact dermatitis” means that the skin reacts to something which it has come into contact with. This term is very general and describes all kinds of reactions which the skin can have. One of my favorites is redness and swelling of the skin around the eyes in little girls attempting to use their mother’s makeup, but the resin can be present on clothes, pets, or tools.
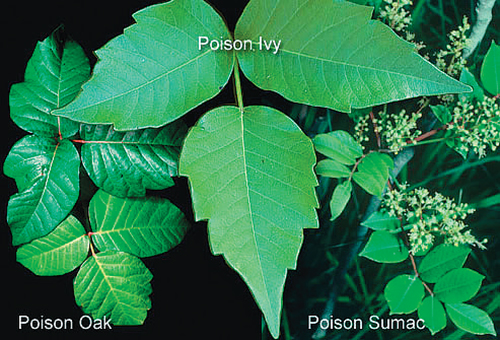
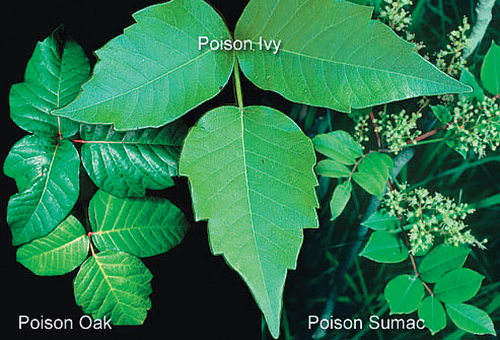
The poison ivy plant occurs in all parts of the United States as a shrub or vine, frequently on fences. Poison oak is an upright shrub present on the west coast and poison sumac is a shrub or a tree found east of the Mississippi. When the resin from these plants comes into contact with the skin of a person who is sensitized, there is a reaction which can take about 48 hours to appear. It usually starts as an area of redness with some itching quickly followed by the formation of linear blisters or vesicles. In severe exposure or severe sensitivity the face may become swollen, especially around the eyes. The presence of itching and subsequent scratching leads to skin breakdown with the possibility of bacteria present on the skin to cause an infection. I have found the face to be the most vulnerable area.
Treatment is aimed at limiting the exposure in order to reduce the inflammation. All clothes should be removed and the body bathed with soap immediately, preferably in the first 15 minutes. Children who have not been bathed properly will scratch one area which has the resin and deposit it onto another area of the body. The use of lotions, like calamine to minimize itching is recommended. Topical antihistamines and numbing creams are not useful and can make the skin worse. Oral antihistamines, like Benadryl, can help tremendously. Rarely is the use of intravenous antibiotics and steroids necessary, but with generalized reactions, severe exposures, or prolonged reactions, the use of steroids may become warranted. It is important to note that the use of steroids should not be for a short period of time but for a full week, tapering off for at least a week more.
It has been said that the best treatment is prevention. This could not be truer when it comes to poison ivy, oak or sumac. Barriers can be effective in preventing exposure—the use of long pants, boots, and gloves while gardening can be helpful, especially as far as sensitive people are concerned. Since the resin has to come into contact to cause a reaction and this requires some time, it makes sense that the best prevention is good old soap and water.
I learned how to be a doctor from medical school and residency. I learned how to be a good mother and a practical doctor from my grandmother. Even in a country where water was scarce, children playing in the outdoors must come in and remove clothing and wash. Practical advice from a practical woman who unfortunately never saw the impact her advice actually had.
If you have any questions you want answered, please address them to Dr. Giuseppina Benincasa-Feingold at “askthedoctor@jewishlinkbc.com.”
By Dr. Giuseppina Benincasa-Feingold